Protes, hernias, osteochondrosis - when they are diagnosed, patients immediately hurry to the surgeon without considering conservative methods of treatment, but this is wrong.
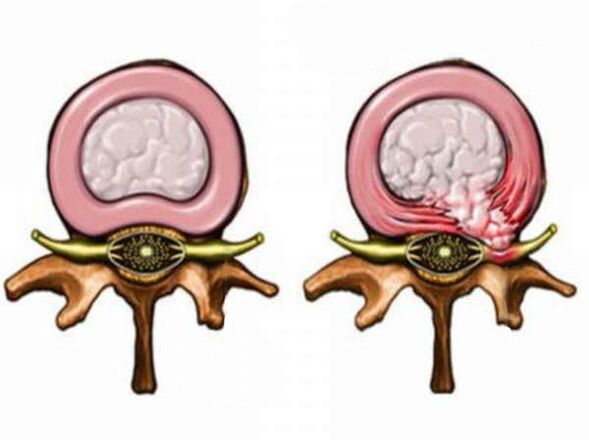
According to statistics, 84% of people at least once in their lives hurt.The spine and the surrounding muscles are part of the musculoskeletal system.Consequently, their damage is often accompanied by pain, which can occur after tilments or turns of the head and body and weaken at rest.Anatomically, the spine is represented by alternating vertebrae and intervertebral discs.The latter over time are subject to the degeneration process, which leads to the formation of protrusions and hernias.These structures can themselves cause pain, and can cause pain by compressing neighboring structures - nerve roots and ligaments of the spine.In some cases, they can cause stenosis (narrowing) of the spinal canal (space in which the spinal cord is located).
Among other things, the vertebrae are connected by pair facet joints, the structure is more rigid than the intervertebral disk.Their damage in 15-65% of cases causes back pain.Up to 30% of the lower back pain is due to the lesion of the sacral and illegal joint-a paired structure connecting the sacrum and bones of the pelvis.Ultimately, any irritation increases the tone of the muscles around, which over time causes a separate myofascial syndrome.
As a rule, physical activity leads to back pain, especially in cases where it is expressed or intense, or when it is produced in an unnatural pose, or when it is associated with a long stay in a forced position, for example, behind the wheel of a car or at a desktop.The body weight and physical training of a person are of great importance, since the severity of the load is always relative.
What are the reasons for its development?
It is impossible to unequivocally call the causes of the development of osteochondrosis, but a number of factors that contribute to the occurrence of this disease can be indicated: poor physical development, a violation of metabolism in the body, genetic predisposition, improper posture, prolonged stay in one pose (for example, before the computer monitor), hypodynamia, and excessively soft bed, flat feet.As a rule, these reasons are combined with irrational nutrition.
What to do if there are pain in the back?
The most important rule is not to self -medicate!
Initially, it is necessary to come to an appointment with a neurologist or neurosurgeon.To establish an accurate diagnosis, a comprehensive examination of the patient is necessary, necessarily including radiography of the spine and tomography (magnetic resonance or computed x-ray. The purpose of this or that study should be carried out only by the attending physician based on a specific clinical picture.
The drug care of osteochondrosis of the spine includes not only the removal of the pain syndrome, but also, if possible, the elimination of the root causes.The doctor prescribes complex therapy (drug therapy, physiotherapy, acupuncture, balneotherapy)
Complex therapeutic care for osteochondrosis includes power and lifestyle correction (healthy and active lifestyle, the optimal volume of physical education), purpose, in some cases - drugs of chondroprotectors that improve the condition of cartilage tissue.
The main indication for surgical treatment for degenerative-dystrophic spinal disease is the inefficiency of conservative drug therapy for 4-6 weeks, unconscious of pain, as well as increasing weakness in the legs, which in a number of cases may be accompanied by urinary incontinence.Untimely and improper treatment in such situations can lead to a number of undesirable consequences and complications, up to disability.
Back pains are recognized as the most common.Experts explain this to the features of human anatomy.The thing is that the spine is subject to loads throughout a person’s life: from the very moment he rises to his feet in childhood until his death.The spinal column wears out, and sooner or later problems with it arise in almost everyone.The most common diagnoses that are made with back pain: “osteochondrosis” and “radiculite”, while often patients put them themselves and prescribe treatment themselves, without seeking advice to doctors.However, even for these diagnoses, which, it would seem, everyone is in hearing, there are often reasons that only an experienced specialist can determine.
What hurts there?
In the vast majority (about 95%), the pain is associated with muscles, ligaments and joints.The people are called to pull the back.These pains are unpleasant, but non -hazardous and in most cases pass on their own in 2-3 days.
3-4% of pains are associated with radiculopathy (radiculitis) - damage to the spinal root.It is usually damaged by a hernia.The pains disappear when the edema that arose due to compression passes.
1-2% of the back pain is caused with injuries or inflammatory diseases of the spine, oncological processes, diseases of the cardiovascular system or the gastrointestinal tract, in which the pain syndrome can go into the back.This is the most dangerous type of back pain.To exclude such pathologies, be sure to consult a doctor.
You can’t delay
The main indicator that you need medical care is the regularity of pain.If you are twisted from time to time, most likely there is nothing wrong.If the pain of low or medium intensity haunts you relentlessly, you can not hesitate.It is urgent to consult a doctor if the pain is accompanied by a temperature rise or pain grows against a background of treatment.
Types of pain
Doctors distinguish 3 types of pain, which most often make themselves felt in the back.The doctor’s task is to accurately determine what kind of pain the patient is concerned about the patient who contacted him, because each of them will be treated exclusively in his own way.
Nociceptive painOr, more simply, pain in the receptors - in the skin, muscles, ligaments, joints - is considered the most common.The reasons that cause it in x -rays or using computed tomography are usually not visible.In this case, the specialist makes the diagnosis based on the symptoms that the patient talks about.The causes of muscle spasm can be, for example, physical activity, when a person lifted something heavy, leaned sharply, or a temperature difference (a common example-purged air conditioning).This type of pain is treated with two types of medicines.
Acute pains are treated with painkillers of anti -inflammatory drugs and drugs relaxing muscles.In this case, there can be no other therapy.When the pain syndrome is removed, we recommend that the patient strengthen muscles with physical education.This is the treatment and the prevention of the disease for the future.
Physical exercises not only help strengthen muscles, but also contribute to the production of endorphins, as well as serotonin and norepinephrine in the body.These substances increase the pain threshold of a person and remove depressive mood.
Neuropathic painOr the pain of the nerve, the people are more known as radiculitis.This type of pain in humans occurs, in particular, when the vertebral hernia becomes large and clamps the nerve endings.At the same time, experts warn patients and the entire professional community against improper diagnosis in cases where the X-ray and using MRI turns out that hernia or any other type of spinal wear is available, but it is not so significant to affect the nerve.It is necessary to carefully understand the true cause of pain.It is possible that a muscle spasm is to blame, and this type of pain is completely different, and treatment will also differ for it.What is considered to be osteochondrosis is not only not manifested by pain, but also the norm.
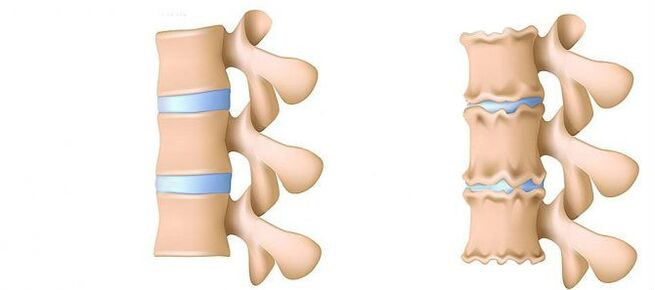
Osteochondrosis is a sign of aging of the body.But "osteochondrosis" and "pain" are not the same.Since there are practically no nerve endings in the bone tissue, the protrusion (the initial stage of the hernia of the intervertebral disc. - Auth.) Or a hernia cannot hurt.Even studies were conducted: MRIs were done groups of people - they chose, mainly those who had never addressed a doctor with complaints about back pain, but they found hernia and osteochondrosis.
In addition, the doctor gives examples when patients received treatment - and they took place, despite the fact that osteochondrosis remained in the picture.Osteochondrosis today is a concept that is used locally.
There are countries where the word "osteochondrosis" is not used at all.Last year, they officially said that this diagnosis was made by past generation neurologists.Abroad, when the patient comes to the reception and says that his back hurts, he is diagnosed with a nonspecific pain in his back, but it is understood that a person gave a load on the muscles.
Confirmation that the pain is caused precisely by radiculitis, and not with spasm, for specialists, the symptom in the form of pain in the back of the back, which give the nerve in the leg, is most often for specialists.
The cause of nerve pain can also be complications that are caused by diabetes and herpes.In diabetes mellitus, patients often complain of pain, as this disease damages the nervous system.The postherpetic neuralgia is characterized by strips of rash along the damaged nerve and, accordingly, pain.There are special drugs for the treatment of nerve pain.
For the treatment of neuropathic pain, anti -epileptic and antidepressants are used.The name of drugs of this orientation of patients, I must say, often scares, so it is important for them to explain that it is antidepressants that increase the pain threshold.These are pain treatment standards.
Psychogenic painor chronic.This type of pain is not caused by physical changes in the human body, his mental state changes.Symptoms torment the patient in this case for a long time.At the same time, it hurts, as a rule, not only the back.
It happens that people come and say everything-my head, back-constantly. You ask: something heavy raised? No! And there is no clear localization. In this case, we can conclude that the patient has reduced the pain threshold and an analyzer of pain, which is in the brain, constantly makes itself felt. It can cause pain in such a patient: overwork, stress, a feeling of fear.
Anesthetic drugs in this case will not help.Specialists usually prescribe antidepressants, physical education to patients with chronic pain, but sometimes it is enough to find a reason using a psychologist or psychiatrist.
A young woman who complained about back pain: six months, he says, was tormented.I recommended that she go to a psychologist and physical education.A few days later she again came completely healthy without taking any medicine.The psychologist helped her understand that the cause of stress pain: she had family problems, physical education helped to relax.
At homeThe most effective remedy is anti -inflammatory oral drugs.Just do not overdo it - they are safe only for the first time.With prolonged use, such drugs can cause ulcers and bleeding in the gastric mucosa.Traditional home treatment - non -steroidal ointments - can only be used as an additional measure.They are harmless, but ineffective.Carsset also gives relief - fixation unloads the spine, relieves spasms and limits sharp movements.Only the corset should be ordinary - elastic, not warming up.
If the treatment has no effect for three days, you should consult a doctor who will make the blockade with anti -inflammatory injections.Due to the removal of spasms and relaxation of muscles, the pain leaves immediately and often forever.
Forbidden!
Bath and massage under the strict prohibition.They enhance edema and pain.
Contact manual therapists in the newspaper.Manual therapy is the area where each specialist accounts for three hundred charlatans.If you really want to find a good doctor, you should contact certified clinics where graduate specialists work.
It is important to immediately correctly determine the tactics of treatment.This should be done by a neurologist or neurosurgeon.It is dangerous to treat your back yourself.30% of patients of the neurosurgical department tried home treatment methods and this brought themselves to a hospital bed.
When pills do not help
If the drug treatment prescribes a therapist or a neuropathologist does not give results within 3-6 months and the pain continues to torment the patient, the doctor is obliged to pass on the patient to another specialist.In some situations, physiotherapy can provide significant assistance.It is suitable for the first two types of pain: in receptors and nerves.Physiotherapy is prescribed to those patients who have an allergy to medicines or stomach problems.
Because of this, the treatment passes, but there is no effect, patients often come to us severe, with depression, so we approach their treatment multidisciplinary, with the involvement of various specialists: neuropathologists, psychologists, physiotherapists, neurosurgeons.
Among the methods that domestic physiotherapists are used, borrowed from Russian colleaguesintracanic electrical stimulation.Its principle is that through a disposable special needle-electrode, bypassing the skin barrier, to supply current, directly in the pain focus.Diagnoses in which this procedure is prescribed, including protrusion and hernia.The procedure, according to experts, is comfortable and does not require pain relief.The effect, as a rule, is felt after the first procedure.In total, they are assigned from 3 to 6.
In addition, it is usedLaser therapy.This technique is also convenient in that it can be prescribed to patients with various stimulants, including cardio- and is not worried that the failure will occur.The laser is used not only for the treatment of diseases associated with the problems of the spine, but also as the treatment of complications of diabetes and herpes sugar, which were already discussed.
The laser promotes good healing.In addition, the device improves microcirculation in the spine itself, and due to this, the power of the disks improves.As a result, edema and inflammation are removed, and pain, respectively, goes away.
Blockade
Such a thing as "blockade" in medicine is not new.With severe pains, since Soviet times, patients were prescribed injections in the area where the pain focus is directly located.Since then, little has changed in the precinct clinics.Meanwhile, in accordance with international recommendations, these procedures must be performed exclusively under control, using special equipment that allows you to monitor the process in real time.The consequences of an unsuccessful injection can be very different: in the best case, the medicine, introduced not to where necessary, will not give the necessary effect, in the worst - this is fraught with serious complications.
The introduction of the drug should be carried out under radiological control: fluoroscopy, CT, MRI, ultrasound, because the drug is administered purposefully into the zone where the source is of pain.In the event that the doctor gets the wrong way, this is fraught with both the patient’s breathing stop and total spinal anesthesia.
The essence of the blockade is that the introduced medicine of several months to six months prevents the spread of the impulse through the nerve, which is involved in the nervous pulse.Although this procedure does not guarantee a constant effect, it significantly improves the patient’s quality of life: a person temporarily forgets about pain, can sleep calmly or go about his business.
Operation - elimination of pain
When the medicines do not help - neither pills nor injections, when physiocracy is ineffective, neurosurgeons come to the rescue.Modern technologies allow these experts to return to life without pain of patients who suffer from it for not one year in a row.There are many methods: from manipulations with the most minimal intervention in the body to complex surgical operations with vertebral prosthetics.
With hernias that pinched the nerve, the so -called one of the most common and effective methods is recognizedRadio frequency ablation.In fact, this is a kind of blockade, only instead of a medicine that relieves pain only for a while, an electric current is used that can completely solve the problem.Often, ablation is done after blockade, thanks to which doctors receive a clear understanding of which nerve it is necessary to influence.The procedure is provided both on a paid basis and by quota.
The procedure is carried out within 20 minutes.It is called an operation, but in fact it is a surgical manipulation that is done under local anesthesia, necessarily under the control of special devices.First, the pain syndrome is reproduced and, if the patient confirms that this is exactly the pain that he usually experiences, we give a pulse discharge - and the pain, so to speak, is disconnected.
In special cases, methods are usedneurostimulationsAmong them is the implement of the electrode.The patient is performed: the surgeon puts a small device in the focus of pain, which will suppress pain impulses in real time.Patients receive this procedure by quota.
There are times when they have already made various types of surgical interventions, but the pain syndrome has been preserved to one degree or another, then we put a stimulant - first in test mode, and if the desired effect is achieved, then we put it for good.This is an operation that is carried out with a small cut.The only thing is that the patient will need to come periodically for test control.
What we risk
The risk of the operation, due to which it is postponed or refused at all, many patients consider it very exaggerated.In neurosurgery, there are technologies that allow you to accurately calculate the effectiveness of the operation and what symptoms will disappear after it and which will remain.
The probability of renewal of pain after surgery does not exceed 1–1.5%.Herbs in other places can really appear, but this is not a complication, but the spread of the disease, which is often found in young undisciplined patients.As soon as the pain leaves, they return to the usual lifestyle: they drive behind the wheel, resume training.And this is categorically impossible to do.
Is osteochondrosis to blame for everything?
Osteochondrosis is a chronic degenerative-dystrophic change in the intervertebral space.All people over 25 years old have signs of osteochondrosis.It is impossible to avoid osteochondrosis, but you can protect yourself from its complications, which cause back pain.
Why so, and not otherwise?
Do I need to spend time, effort and money on treatment: tablets, injections, physiotherapy, if you can immediately do a small operation and get rid of pain once and for all?- Patients have been asking this question more and more often.The answer is usually unambiguous: yes, you need!The thing is that with accurate diagnosis and proper treatment, units reach operations.The rest get rid of pain in the first stages of assistance - on average, 30% of patients at each stage are output.
A mistake when people, having seen a protrusion or hernia in the picture, immediately run to the surgeon, bypassing the specialists of the previous stages of assistance.In cases where the changes are insignificant, the operation is not required.Moreover, with the right lifestyle - engaged in physiotherapy exercises, swimming, monitoring the weight of his body - a person with the so -called osteochondrosis can feel healthy and not experience pain.
It is important that at each stage the patient has an accurate diagnosis and the correct treatment is prescribed.This can only be achieved collegial.It is also proposed, on the example of foreign experience, to introduce a new specialization, such as an algologist, is a kind of therapist specializing in pain, a doctor who has the knowledge of a neurologist and anesthetist interventionist, capable of treating, without led to surgery, but if surgical intervention will nevertheless inevitably convey the patient to neurosurgeons.



































